Infiltrations are injections placed at different body structures in order to either diagnose or treat a certain cause for pain.
Diagnostic Infiltrations
Diagnostic infiltrations are a valuable tool in order to pinpoint the cause of pain. A small amount of a local anesthetic is carefully injected at the suspected source of pain.
Therapeutic Infiltrations
Therapeutic infiltrations are used for targeted treatment with a drug (or autologous blood). Depending on the pain origin we infiltrate joints, discs, nerves, ganglions, muscles and fascia. We use local anesthetic, cortisone, hyaluronic acid, Botox or PRP (platelet rich plasma), depending on the underlying cause.
Examples
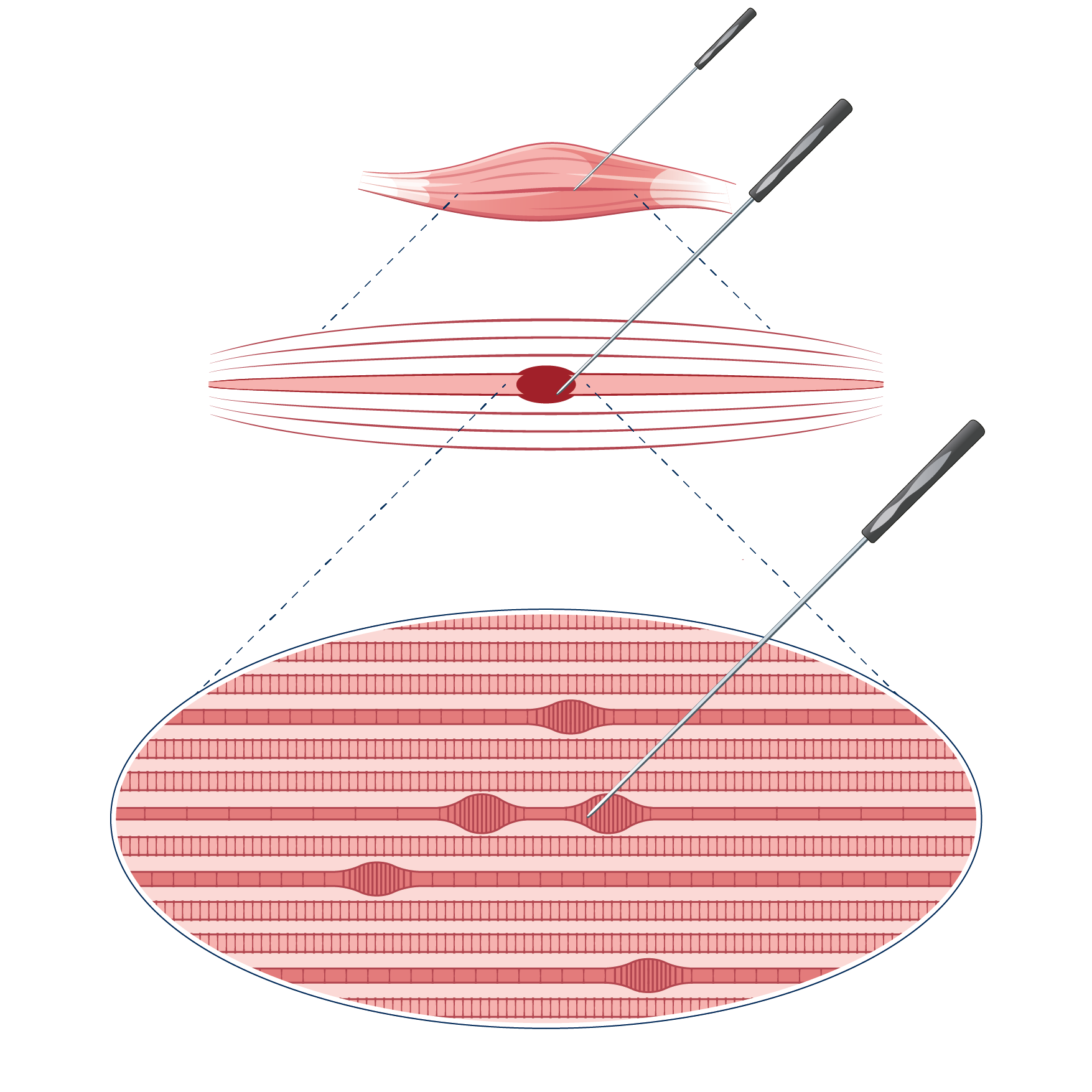
Trigger point infiltrations and dry needling
Trigger points within the musculature are points of unwanted continuous contraction in certain muscle filaments. They typically originate from overuse or strain due to bad posture. Another common cause for trigger points is muscle strain due to whiplash trauma. Trigger points can range from painless conditions to immobilizing pain – depending on the extent of muscle fibers involved and other cofactors.
According to research there is an acidic milieu with low oxygen values within trigger points. Without oxygen there is no energy source for ATP (Adenosintriphosphate) which is essential for the release of tightly contracted muscle fibers.
Trigger point infiltrations und Dry Needling as therapy
Already in the 1940s physicians discovered that infiltrating trigger points with local anesthetic can lead to long lasting if not permanently pain free conditions. Furthermore, a similar effect was observed when injecting physiologic salt solution (NaCl). Later it was discovered that also needles alone resolve trigger points, at which point the idea of dry needling was “born”: trigger points can be released by puncturing the muscle with a needle alone (dry needling).
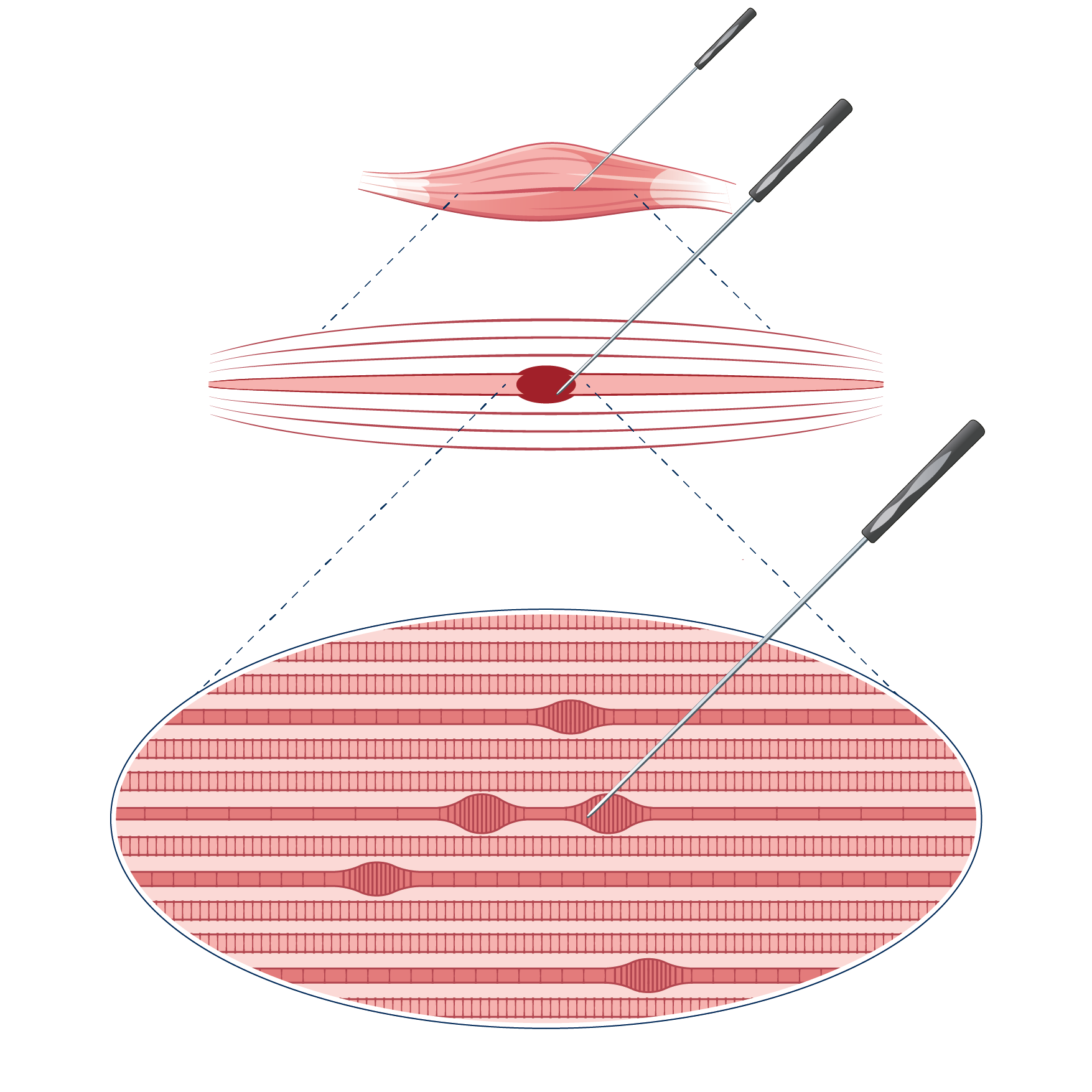
Needle puncture can increase the blood flow and thus oxygen concentration within trigger points, leading to a release of contracted muscle fibers.
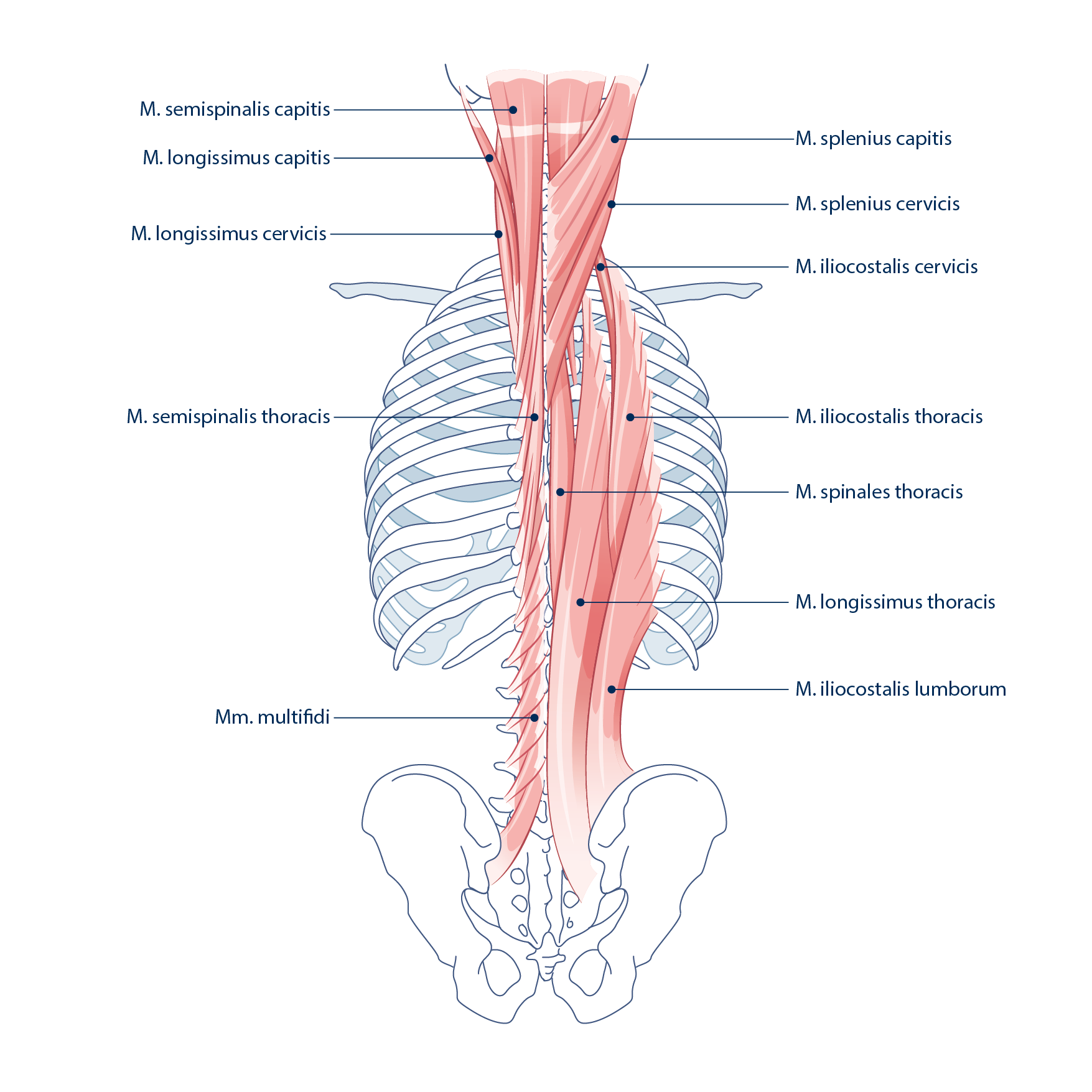
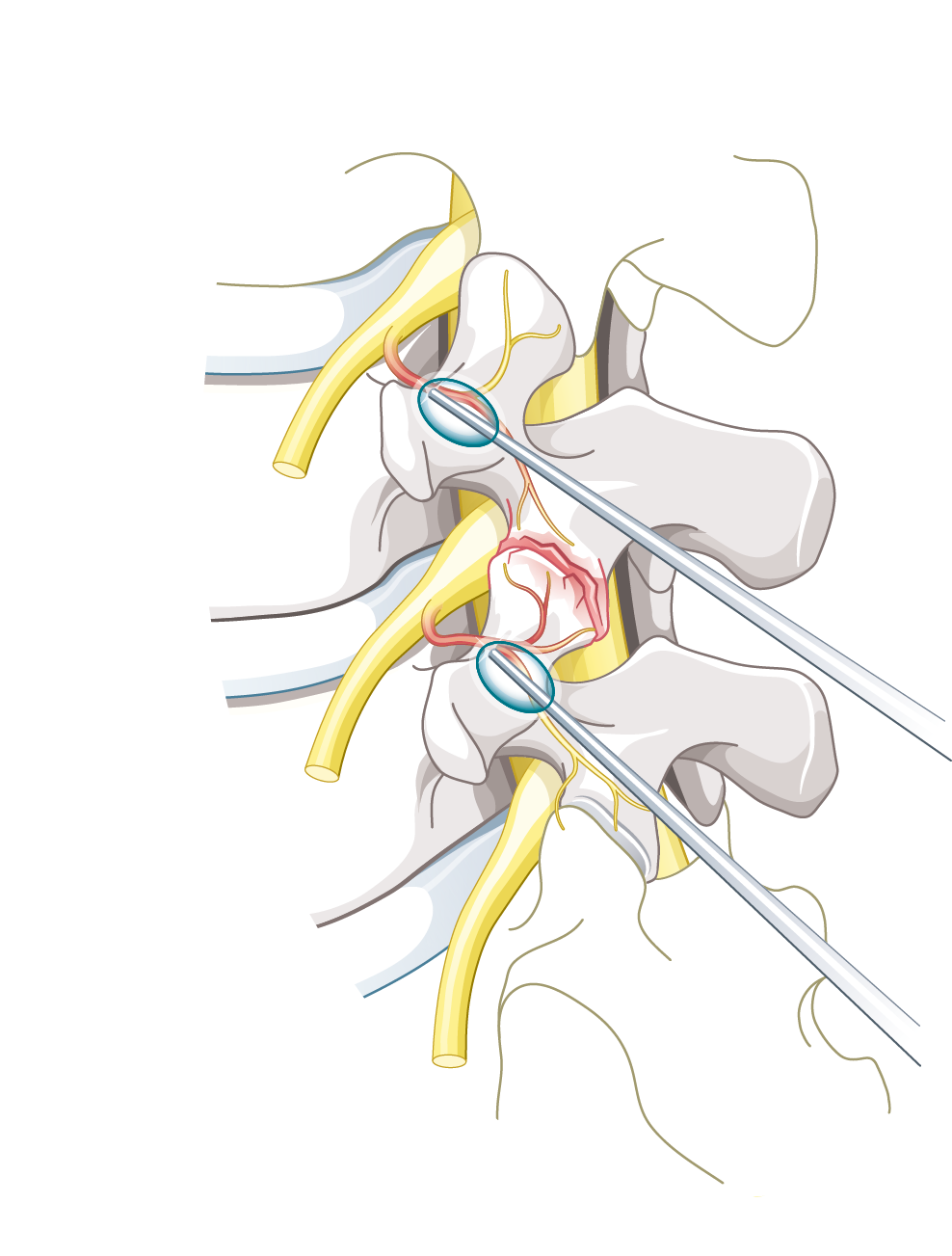
Advances technique – advantage of ultrasound guided dry needling
With traditional dry needling (without ultrasound guidance) it is safe to treat superficial muscle groups and muscles that can be easily reached. Deep muscles in proximity to the spinal cord or close to the lungs are difficult to treat. Treatment of the erector spinae muscle close to the spine for example is more effective with ultrasound guidance.
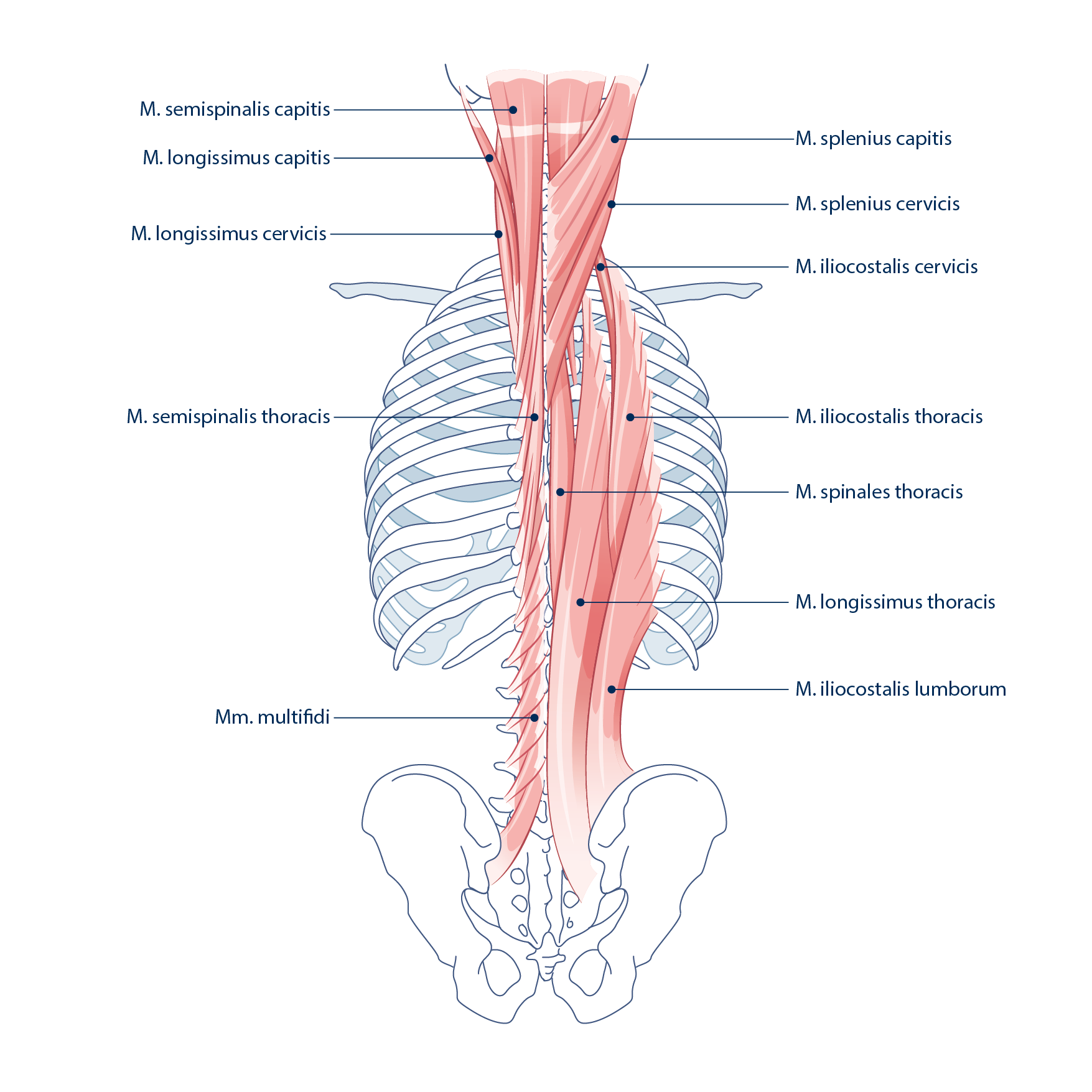
Modern ultrasound machines are able to show the structures which need to be treated as well as tissues (i.e. lungs, blood vessels, epidural space) that need to be avoided.
With ultrasound the safety and accuracy is improved which allows for optimal treatment that was previously not possible. Experience and the necessary infrastructure can provide pain alleviation for many patients who have suffered for years.
![]()
Autohemotherapy
Definitions
For autohemotherapy two different abbreviations are in use: ACP (autologous conditioned plasma) or PRP (platelet rich plasma).
How does autohemotherapy work?
Platelet rich plasma (PRP) contains messengers which can propagate regeneration and healing in different tissues. Injured tissue goes through complex, intricate healing processes. Blood proteins – originating from platelets and plasma – interact with surrounding cells and are thus responsible für these healing processes. Therefore, these active substances are generated from the patient’s own blood and can be targeted and concentrated where tissue needs healing. This technique has been improved constantly over recent years.
When to apply autohemotherapy?
Infiltration with PRP is applied when the main focus is on tissue regeneration and not on suppression of inflammation.
How does autohemotherapy work?
A small amount of blood is drawn from an arm vein. With a special process (centrifugation) PRP is separated and the active regenerating substances are released from cells and now contained within PRP. PRP can be injected directly into injured muscles, tendons and joints. All this is done under sterile conditions and with especially developed syringes.
Onabotulinumtoxin A (Botox))
Botox Injections block chemical signals from nerve endings in the muscles. This prevents the muscle fibers from moving. Botox injections can help reduce migraine attacks when targeted to certain muscle groups. Furthermore Botox infiltrations can also be applied successfully when treating patients who are suffering from muscle dystonia and in cases of unwanted increased muscle tonus.
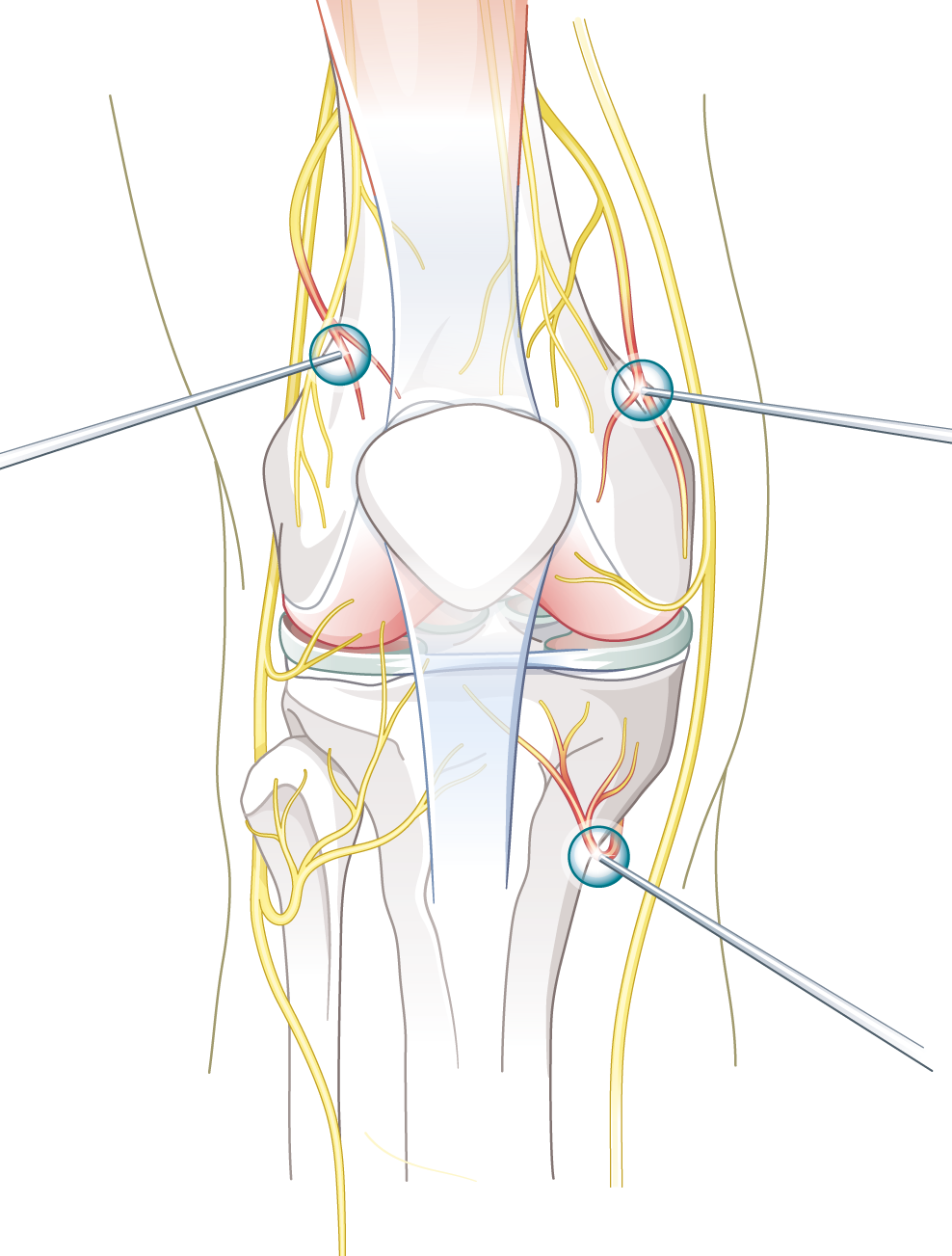
Another treatment option is using the pain modulating effect of Botox at the nerves (and not the nerve endings). In this case the nerve is located with ultrasound in order to carefully inject Botox round the nerve.
Neural therapy
With neural therapy local anesthetic is injected around the nerve in an attempt to temporarily anesthetize the nerve. Even though the anesthesia is temporary, the procedure can lead to permanently reducing the nerve’s irritation. This effect can be compared to rebooting a computer. The method is especially effective if there is a neuroplastic pain component.
Also through «hydrodissection» – a side effect by separating tissue layers from one another through injecting a solution – can have a therapeutic effect. This treatment is especially effective with nerve compression and fascia are stuck together.